Description
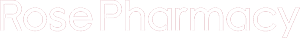
Ziac 5.0/6.25Mg Tablet
Description :
Each tablet contains bisoprolol hemifumarate 2.5, 5 or 10 mg, and hydrochlorothiazide 6.25 mg.
Indications / Uses :
Treatment of hypertension.
Administration :
May be taken with or without food.
Contraindications :
Bisoprolol: Severe asthma or severe chronic obstructive airway disease; heart failure not sufficiently controlled by therapy; cardiogenic shock; sick sinus syndrome (including SA block); 2nd- or 3rd-degree AV block (with no implanted pacemaker); significant bradycardia (heart rate <50 bpm); Prinzmetal’s angina (pure vasospastic angina and single-agent therapy); pheochromocytoma (except after prior a-receptor blocker therapy); severe forms of Raynaud’s phenomenon and severe peripheral arterial disease; hypotension; hypersensitivity to bisoprolol; concurrent use of floctafenine (see Interactions); concurrent use of sultopride (see Interactions); bisoprolol should not be combined with amiodarone (see Interactions).
Hydrochlorothiazide: Hypersensitivity to sulfonamides; severe renal impairment (creatinine clearance =30 mL/min). Hydrochlorothiazide should not be combined with lithium or non-antiarrhythmic drugs that may produce torsade de pointes, ventricular tachycardias (see Interactions).
Special Precautions :
Bisoprolol: Cessation of Therapy: Therapy should not be stopped or interrupted abruptly, especially in patients with ischemic heart disease, but rather be tapered over approximately 1-2 weeks, at the same time substituting appropriate therapy if necessary, to prevent exacerbation of anginal symptoms.
Asthma and Chronic Obstructive Airway Disease: ?-Blockers may be used in mild forms of asthma or COAD using a ?1-selective adrenoceptor-blocking agent and a low starting dose. Pulmonary function testing is recommended before the start of therapy. An asthma attack/bronchospasm that might occur during therapy may be controlled with ?2-agonists.
Cardiac Failure: Patients with compensated cardiac failure who require ?-blocker therapy may be administered bisoprolol using a very low starting dose, to be increased gradually with close medical monitoring.
Bradycardia: If heart rate at rest falls below 50-55 bpm and the patient experiences bradycardia-related symptoms, the dosage will have to be reduced.
1st-Degree AV Block: Having negative dromotropic activity, ?-blocker should be used cautiously in patients with 1st-degree AV block.
Prinzmetal’s Angina: ?-Blockers may increase the frequency and length of vasospastic episodes in patients with Prinzmetal’s angina. A cardioselective ?-blocker may be used in minor or mixed forms if a vasodilator is used concurrently.
Peripheral Arterial Disease: ?-Blockers may aggravate the symptoms of PAD (Raynaud’s disease or syndrome, chronic obliterative arteritis or artery disease of the legs). Such patients should preferably be prescribed a cardioselective ?-blocker with partial agonist activity, to be administered cautiously.
Pheochromocytoma: ?-Blocker use in hypertension due to treated pheochromocytoma requires close blood pressure monitoring.
Diabetics: Diabetic patients should be informed of the risk of hypoglycemic episodes and of the increased need for careful home glucose monitoring in the initial phase of therapy. The warning signs of hypoglycemia, particularly tachycardia, palpitations and sweating, may be masked.
Psoriasis: There have been reports of ?-blockers being associated with worsening of psoriasis, so patients with psoriasis should receive bisoprolol only if clearly needed.
Allergic Reactions: In patients at risk of severe anaphylactic reaction to whatever allergen, particularly when using iodine-containing contrast materials or floctafenine (see Interactions) or during specific immunotherapy (desensitization), ?-blockers may aggravate the anaphylactic reaction and cause unresponsiveness to the usual doses of epinephrine used to treat allergic reactions.
General Anesthesia: ?-Blockers are liable to attenuate reflex tachycardia, increasing the risk for hypotension. Continuation of ?-blocker therapy reduces the risk of arrhythmia, myocardial ischemia and hypertensive episodes. The anesthesiologist should be informed that the patient is receiving ?-blocker therapy.
If interruption of therapy is considered necessary, withholding the ?-blocker for 48 hrs is considered adequate to restore responsiveness to catecholamines. However, ?-blocker therapy cannot be interrupted in the following settings: In patients with coronary artery disease, it is advisable to continue therapy until the surgical procedure, given the risk associated with abrupt cessation of ?-blocker therapy. In an emergency setting or if the ?-blocker cannot be stopped, the patient should be protected against vagal predominance by adequate atropine pre-medication, to be repeated as necessary. Anesthetic agents should be selected to minimize depression of myocardial function, and blood loss should be compensated.
Anaphylactic risk should be taken into account.
Thyrotoxicosis: ?-Blockers are liable to mask the cardiovascular signs of hyperthyroidism.
Competitive Athletes: Competitive athletes should be informed that Ziac contains a drug that may give a positive reaction in doping tests.
Hydrochlorothiazide: Fluid and Electrolyte Balance: Plasma Sodium: Plasma sodium should be determined before and periodically during therapy. Any diuretic therapy may give rise to hyponatremia with serious consequences in some cases. As hyponatremia may initially be asymptomatic, periodic monitoring is indispensable and should be more frequent in high-risk populations, ie the elderly and patients with cirrhosis of the liver (see Side Effects and Overdosage).
Plasma Potassium: Potassium loss resulting in hypokalemia is the greatest risk associated with thiazide diuretics and related drugs. The risk of hypokalemia (<3.5 mmol/L) should be anticipated in certain high-risk populations, ie patients who are elderly and/or malnourished and or take multiple drugs, liver cirrhosis patients with edema and ascites, and patients with coronary artery disease or heart failure, where hypokalemia increases the cardiotoxicity of digitalis glycosides and the risk of cardiac arrhythmia. Also at risk are patients with long QT syndrome, either congenital or iatrogenic. Hypokalemia (as well as bradycardia) facilitates the development of severe arrhythmias, particularly torsade de pointes, which may be fatal. More frequent plasma potassium monitoring is indicated in all the previously mentioned populations, starting in the week after initiation of therapy.
Plasma Calcium: Thiazide diuretics and related drugs may reduce urinary calcium excretion, resulting in mild, transient hypercalcemia. Significant hypercalcemia may be related to undiagnosed hyperparathyroidism. Therapy must be interrupted before performing parathyroid function test.
Blood Glucose: In diabetics, blood glucose must be monitored, especially in the presence of hypokalemia.
Uric Acid: In patients with hyperuricemia, the risk for attacks of gout may be increased. Dosage should be adjusted as a function of uric acid plasma concentrations.
Kidney Function and Diuretics: Full benefit from thiazide diuretics can be derived only if kidney function is normal or almost normal (serum creatinine <25 mg/L or 220 micromole/L in adults). In elderly patients, serum creatinine needs to be corrected for age, weight and gender using Cockroft’s formula for instance:
CrCl = (140 – age) x weight/0.814 x serum creatinine
Where age is indicated in years; weight in kg; and serum creatinine in micromole/L.
The previous formula gives CrCl for elderly male subjects and needs to be corrected for elderly female subjects by multiplying by 0.85.
Hypovolemia secondary to diuretic-induced water and sodium loss at the start of therapy reduces glomerular filtration, which may result in BUN and serum creatinine increases. The transient functional renal impairment is insignificant in patients with normal kidney function but may worsen preexisting renal insufficiency.
Combination with Other Antihypertensive Drugs: It is advisable to reduce the dosage when Ziac is combined with another antihypertensive, at least in the initial phase of therapy.
Competitive Athletes: Competitive athletes should be informed that Ziac contains a drug that may give a positive reaction in doping tests.











Reviews
There are no reviews yet.