Description
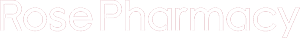
PROVERA 10MG TABLET
Description :
Provera contains medroxyprogesterone acetate, a derivative of progesterone, as its active ingredient. Medroxyprogesterone acetate is active by the parenteral and oral routes of administration. It is a white to off-white, odorless crystalline powder that is stable in air and that melts between 200?C and 210?C. It is freely soluble in chloroform, soluble in acetone and dioxane, sparingly soluble in alcohol and methanol, slightly soluble in ether and insoluble in water.
Medroxyprogesterone acetate is pregn-4-ene-3,20-dione,17-(acetyloxy)-6-methyl-,(6a).
Indications / Uses :
Gynecology: Treatment of endometriosis; treatment of menopausal vasomotor symptoms; diagnosis of primary amenorrhea; diagnosis and treatment of secondary amenorrhea; treatment of dysfunctional (anovulatory) uterine bleeding; opposition of endometrial effects of estrogen in menopausal women being treated with estrogen (hormone therapy).
Oncology: Recurrent and/or metastatic breast cancer; endometrial cancer, renal cancer; metastatic prostate cancer; anorexia and cachexia syndrome.
Administration :
May be taken with or without food.
Contraindications :
Hypersensitivity to MPA or to any component of Provera eg lactose monohydrate, maize starch, sucrose, liquid paraffin, talc and calcium stearate.
Known or suspected pregnancy.
Undiagnosed vaginal bleeding.
Severe liver dysfunction.
Gynecology: Known of suspected malignancy of the breast.
Undiagnosed vaginal bleeding; liver dysfunction or disease.
Pregnancy: MPA is contraindicated in women who are pregnant.
Some reports suggest under certain circumstances, an association between intrauterine exposure to progestational drugs in the first trimester of pregnancy and genital abnormalities in fetuses.
If the patient becomes pregnant while using this drug, the patient should be apprised of the potential hazard to the fetus.
Special Precautions :
General: Unexpected vaginal bleeding during therapy with MPA should be investigated. MPA may cause some degree of fluid retention; therefore, caution should be exercised in treating any patient with a preexisting medical condition that might be adversely affected by fluid retention.
Patients with a history of treatment for clinical depression should be carefully monitored while receiving MPA therapy.
Some patients receiving medroxyprogesterone may exhibit a decrease in glucose tolerance. Diabetic patients should be carefully observed while receiving such therapy.
The pathologist (laboratory) should be informed of the patient’s use of MPA if endometrial or endocervical tissue is submitted for examination.
The physician/laboratory should be informed that use of MPA may decrease the levels of the following endocrine biomarkers: Plasma/urinary steroids (eg, cortisol, estrogen, pregnanediol, progesterone, testosterone); plasma/urinary gonadotrophins (eg, LH and FSH); sex-hormone-binding-globulin.
Medication should not be re-administered pending examination if there is a sudden partial or complete loss of vision or if there is a sudden onset of proptosis, diplopia or migraine. If examination reveals papilledema or retinal vascular lesions, medication should not be re-administered.
MPA has not been causally associated with the induction of thrombotic or thromboembolic disorders, however, MPA is not recommended in any patient with a history of venous thromboembolism (VTE). Discontinuation of MPA is recommended in patients who develop VTE while undergoing therapy with MPA.
Gynecology: Treatment of Menopausal Vasomotor Symptoms/Opposition of Endometrial Effects of Estrogen in Menopausal Women Being Treated with Estrogen (Hormone Therapy) All Formulations: Other doses of oral conjugated estrogens with medroxyprogesterone and other combinations and dosage forms of HT were not studied in the WHI trial (see Pharmacology: Pharmacodynamics under Actions) and in the absence of comparable data, these risks should be assumed to be similar.
Breast Cancer: The use of combined estrogen/progestin by postmenopausal women has been reported to increase the risk of breast cancer. Results from a randomized placebo-controlled trial, the WHI trial, and epidemiological studies (see Pharmacology: Pharmacodynamics under Actions) have reported an increased risk of breast cancer in women taking estrogen/progestin combinations for HT for several years. In the WHI conjugated equine estrogens (CEE) plus MPA trial and observational studies, the excess risk increased with duration of use (see Dosage & Administration). The use of estrogen plus progestin has been reported to result in an increase in abnormal mammograms requiring further evaluation.
Cardiovascular Disorders: Estrogens with or without progestins should not be used for the prevention of cardiovascular disease. Several randomized, prospective trials on the long-term effects (see Dosage & Administration) of a combined estrogen/progestin regimen in postmenopausal women have reported an increased risk of cardiovascular events eg, myocardial infarction, coronary heart disease, stroke and venous thromboembolism.
Coronary Artery Disease: There is no evidence from randomized controlled trials of cardiovascular benefit with continuous combined conjugated estrogen and medroxyprogesterone. Two (2) large clinical trials [WHI CEE/ MPA and Heart and Estrogen/Progestin Replacement Study (HERS) (see Pharmacology: Pharmacodynamics under Actions)] showed a possible increased risk of cardiovascular morbidity in the 1st year of use and no overall benefit.
In the CEE/MPA trial, an increased risk of CHD events (defined as nonfatal myocardial infarction and CHD death) was observed in women receiving CEE/MPA compared to women receiving placebo (37 vs 30 per 10,000 person years). The increase in VTE risk was observed in year 1 and persisted over the observation period (see Dosage & Administration).
Stroke: In the WHI CEE/MPA trial, an increased risk of stroke was observed in women receiving CEE/MPA compared to women receiving placebo (29 vs 21 per 10,000 person-years). The increase in risk was observed in year 1 and persisted over the observation period (see Dosage & Administration).
Dementia: The WHIMS (see Pharmacology: Pharmacodynamics under Actions), an ancillary study of WHI for CEE/MPA, reported an increased risk of probable dementia in postmenopausal women =65 years. In addition, CEE/MPA therapy did not prevent mild cognitive impairment (MCI) in these women. Use of hormone therapy (HT) to prevent dementia or MCI in women =65 years is not recommended.
Ovarian Cancer: Current use of estrogen only or estrogen plus progestin products in post-menopausal women for =5 years, has been associated with an increased risk of ovarian cancer in some epidemiological studies. Past users of estrogen only or estrogen plus progestin products were at no increased risk for ovarian cancer. Other studies did not show a significant association. The WHI CEE/MPA trial reported that estrogen plus progestin increased the risk of ovarian cancer, but this risk was not statistically significant. In 1 study, women who use HRT are at increased risk of fatal ovarian cancer.
History and Physical Exam Recommendation: A complete medical and family history should be taken before the initiation of any hormone therapy. Pre-treatment and periodic physical examination should include special reference to blood pressure, breasts, abdomen and pelvic organs, including cervical cytology.
Oncology: MPA may produce Cushingoid symptoms. Some patients receiving medroxyprogesterone may exhibit suppressed adrenal function. MPA may decrease ACTH and hydrocortisone blood levels.
The physician/laboratory should be informed that in addition to the endocrine biomarkers listed previously, the use of MPA in oncology indications may also cause partial adrenal insufficiency (decrease in pituitary-adrenal axis response) during metyrapone testing. Thus, the ability of adrenal cortex to respond to ACTH should be demonstrated before metyrapone is administered.
Oral Formulations & High-Dose Parenteral Formulations (eg, Oncology Use in Premenopausal Women): Decrease in Bone Mineral Density: There are no studies on the bone mineral density (BMD) effects of orally administered MPA or the high doses of parenteral MPA (eg, for oncology use).
An evaluation of BMD may be appropriate in some patients who use MPA long-term.
Effects on the Ability to Drive and Use Machines: The effect of MPA on the ability to drive and use machinery has not been systematically evaluated.










Reviews
There are no reviews yet.