Description
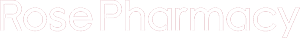
Flixotide 5Mg Nebules
Description :
Diskus: Each 100, 250 or 500 diskus contains salmeterol xinafoate 50 mcg and fluticasone propionate 100, 250 or 500 mcg, respectively. It also contains lactose (which contains milk proteins) as an excipient.
MDI: Each actuation of 25/50 mcg, 25/125 mcg, 25/250 mcg contains salmeterol xinafoate 25 mcg and fluticasone propionate 50, 125 or 250 mcg.
Seretide MDI comprises a suspension of salmeterol and fluticasone propionate in the non-CFC propellant HFA 134a. The suspension is contained in an aluminum alloy can sealed with a metering valve. The canisters are fitted into plastic actuators incorporating an atomizing orifice and fitted with dust caps.
Indications / Uses :
Asthma [Reversible Obstructive Airway Disease (ROAD)]: Regular treatment of asthma may include: Patients on effective maintenance doses of long-acting ?-agonists and inhaled corticosteroids; who are symptomatic on current inhaled corticosteroid therapy; on regular bronchodilator therapy who require inhaled corticosteroids.
Chronic Obstructive Pulmonary Disease (COPD): Regular treatment of COPD including chronic bronchitis and emphysema.
Contraindications :
History of hypersensitivity to salmeterol, fluticasone propionate or any of the ingredients of Seretide.
Special Precautions :
Seretide is not for relief of acute symptoms for which a fast- and short-acting bronchodilator (eg, salbutamol) is required. Patients should be advised to have their relief medication available at all times.
Increasing use of short-acting bronchodilators to relieve symptoms indicates deterioration of control and patients should be reviewed by a physician.
Sudden and progressive deterioration in control of asthma is potentially life-threatening and the patient should be reviewed by a physician. Consideration should be given to increasing corticosteroid therapy. Also, where the current dosage of Seretide has failed to give adequate control of asthma, the patient should be reviewed by a physician.
Treatment with Seretide should not be stopped abruptly in patients with asthma due to the risk of exacerbation, therapy should be titrated down under physician supervision. For patients with COPD, cessation of therapy may be associated with symptomatic decompensation and should be supervised by a physician.
There was an increased reporting of pneumonia in studies of patients with COPD receiving Seretide (see Adverse Reactions). Physicians should remain vigilant for the possible development of pneumonia in patients with COPD as the clinical features of pneumonia and exacerbation frequently overlap.
As with all inhaled medication containing corticosteroids, Seretide should be administered with caution in patients with active or quiescent pulmonary tuberculosis.
Seretide should be administered with caution in patients with thyrotoxicosis.
Cardiovascular effects eg, increases in systolic blood pressure and heart rate, may occasionally be seen with all sympathomimetic drugs, especially at higher than therapeutic doses. For this reason, Seretide should be used with caution in patients with preexisting cardiovascular disease.
A transient decrease in serum potassium may occur with all sympathomimetic drugs at higher therapeutic doses. Therefore, Seretide should be used with caution in patients predisposed to low levels of serum potassium.
Systemic effects may occur with any inhaled corticosteroid, particularly at high doses prescribed for long periods; these effects are much less likely to occur than with oral corticosteroids (see Overdosage). Possible systemic effects include Cushing’s syndrome, Cushingoid features, adrenal suppression, growth retardation in children and adolescents, decrease in bone mineral density, cataract and glaucoma. It is important therefore for asthma patients, that the dose of inhaled corticosteroid is titrated to the lowest dose at which effective control is maintained.
The possibility of impaired adrenal response should always be borne in mind in emergency and elective situations likely to produce stress and appropriate corticosteroid treatment considered (see Overdosage).
It is recommended that the height of children receiving prolonged treatment with inhaled corticosteroid is regularly monitored.
Because of the possibility of impaired adrenal response, patients transferring from oral steroid therapy to inhaled fluticasone propionate therapy should be treated with special care and adrenocortical function regularly monitored.
Following introduction of inhaled fluticasone propionate, withdrawal of systemic therapy should be gradual and patients encouraged to carry a steroid warning card indicating the possible need for additional therapy in times of stress.
There have been very rare reports of increases in blood glucose levels (see Adverse Reactions) and this should be considered when prescribing to patients with a history of diabetes mellitus.
During post-marketing use, there have been reports of clinically significant drug interactions in patients receiving fluticasone propionate and ritonavir, resulting in systemic corticosteroid effects including Cushing’s syndrome and adrenal suppression. Therefore, concomitant use of fluticasone propionate and ritonavir should be avoided, unless the potential benefit to the patient outweighs the risk of systemic corticosteroid adverse effects (see Interactions).
Data from a large US study (SMART) comparing the safety of Serevent, (a component of Seretide) or placebo added to usual therapy showed a significant increase in asthma-related deaths in patients receiving Serevent. Data from this study suggested that African-American patients may be at greater risk of serious respiratory-related events or deaths when using Serevent compared to placebo. It is not known if this was due to pharmacogenetic or other factors. The SMART study was not designed to determine whether concurrent use of inhaled corticosteroids modifies the risk of asthma-related death (see Pharmacology: Clinical Studies under Actions).
It was observed in a drug interaction study that concomitant use of systemic ketoconazole increases exposure to Serevent. This may lead to prolongation in the QTc interval. Caution should be exercised when strong CYP3A4 inhibitors (eg, ketoconazole) are co-administered with Serevent (see Pharmacology: Pharmacokinetics under Actions and Interactions).
As with other inhalation therapy, paradoxical bronchospasm may occur with an immediate increase in wheezing after dosing. This should be treated immediately with a fast- and short-acting inhaled bronchodilator. Salmeterol-fluticasone propionate accuhaler/diskus or evohaler should be discontinued immediately, the patient assessed and alternative therapy instituted if necessary (see Adverse Reactions).
The pharmacological side effects of ?2-agonist treatment eg, tremor, subjective palpitations and headache have been reported, but tend to be transient and to reduce with regular therapy (see Adverse Reactions).
Effects on the Ability to Drive or Operate Machinery: There have been no specific studies of the effect of Seretide on the previously mentioned activities, but the pharmacology of both drugs does not indicate any effect.
Use in Children: There are no data available for use in Seretide in children <4 years.
Use in Pregnancy & Lactation: Administration of drugs during pregnancy and lactation should only be considered if the expected benefit to the mother is greater than any possible risk to the fetus or child.
There is insufficient experience of the use of salmeterol xinafoate and fluticasone propionate in human pregnancy and lactation.
Reproductive toxicity studies in animals, either with single drug or in combination, revealed the fetal effects expected at excessive systemic exposure levels of a potent ?2-adrenoreceptor agonist and glucocorticosteroid.
Extensive clinical experience with drugs in these classes has revealed no evidence that the effects are relevant at therapeutic doses. Neither salmeterol xinafoate or fluticasone propionate have shown any potential for genetic toxicity.
Salmeterol and fluticasone propionate concentrations in plasma after inhaled therapeutic doses are very low and therefore, concentrations in human breast milk are likely to be correspondingly low. This is supported by studies in lactating animals, in which low drug concentrations were measured in milk. There are no data available for human breast milk.
Caution for Usage
Instructions for Use and Handling: Diskus: The diskus is sealed in a foil overwrap. The overwrap provides moisture protection and should only be opened when the patient is ready to use it for the 1st time. Once opened, the foil overwrap should be discarded.
The diskus releases a powder which is inhaled into the lungs.
The device is opened and primed by sliding the lever. The mouthpiece is then placed in the mouth and the lips closed around it. The dose can then be inhaled and the device closed.
A dose indicator on the diskus indicates the number of doses left.
Closed: When the patient takes the diskus out of its box and remove the foil overwrap, it will be in the closed position.
Opened: A new Diskus contains 28 or 60 doses individually protected doses of Seretide, in powder form. The dose indicator indicates the number of doses left.
Each dose is accurately measured and hygienically protected. It requires no maintenance and no refilling.
The dose indicator on top of the diskus indicates how many doses are left. Numbers 5 to 0 will appear in red, to warn the patient when there are only a few doses left.
The diskus is easy to use. When the patient needs a dose, these 5 simple steps should be followed: 1. Open. 2. Slide. 3. Inhale. 4. Close. 5. Rinse.
How the Diskus Works: Sliding the lever of the diskus opens a small hole in the mouthpiece and unwraps a dose, ready to be inhaled by the patient.
When the diskus is closed, the lever automatically moves back to its original position, ready for the next dose when the patient needs it. The outer case protects the Diskus when it is not in use.
1. Open: How to Use the Diskus: To open the diskus, hold the outer case in 1 hand and put the thumb of the other hand on the thumbgrip. Push the thumb away from the patient as far as it will go.
2. Slide: Hold the diskus with the mouthpiece towards the patient. Slide the lever away as far as it will go until it clicks. The diskus is now ready to use. Every time the lever is pushed back, a dose is made available for inhaling. This is shown by the dose counter. Do not play with the lever as this releases doses which will be wasted.
3. Inhale: Hold the diskus away from the mouth. Breathe out as far as is comfortable. Remember to never breathe into the diskus.
Put the mouthpiece to the lips. Breathe in steadily and deeply through the diskus, not through the nose.
Remove the diskus from the mouth.
Hold breath for about 10 sec or for as long as is comfortable. Breathe out slowly.
4. Close: To close the diskus, put the thumb in the thumbgrip and slide the thumbgrip back towards the patient, as far as it will go.
When the diskus is closed, it clicks shut. The lever automatically returns to its original position and is reset. The diskus is now ready for use again.
5. Rinse: Afterwards, rinse the mouth with water and spit it out.
If the patient have been instructed to take 2 inhalations, the diskus must be closed first and then repeat steps 1 to 4.
Remember: Keep the diskus dry.
Keep it closed when not in use.
Never breathe into the diskus.
Only slide the lever when the patient is ready to take a dose.
Do not exceed the stated dose.
Seretide Metered Dose Inhaler: Testing the Inhaler: Before using for the first time or if the inhaler has not been used for a week or more remove the mouthpiece cover by gently squeezing the sides of the cover, shake the inhaler well, and release 1 puff into the air to make sure that it works.
Using the Inhaler:
1. Remove the mouthpiece cover by gently squeezing the sides of the cover.
2. Check inside and outside of the inhaler including the mouthpiece for the presence of loose objects.
3. Shake the inhaler well? that any loose objects are removed and that the contents of the inhaler are evenly mixed.
4. Hold the inhaler upright between fingers and thumb with thumb on the base, below the mouthpiece.
5. Breathe out as far as is comfortable and then place the mouthpiece in the mouth between the teeth and close the lips around it, without biting.
6. Just after starting to breathe in through the mouth, press firmly down on the top of the inhaler to release salmeterol and fluticasone propionate, while still breathing in steadily and deeply.
7. While holding breath, take the inhaler from the mouth and take the finger from the top of the inhaler. Continue holding breath for as long as is comfortable.
8. To take the 2nd puff, keep the inhaler upright and wait about ? a minute before repeating steps 3 to 7.
9. Afterwards rinse the mouth with water and spit it out.
10. Replace the mouthpiece cover by firmly pushing and snapping the cap into position.
Important: Do not rush stages 5, 6 and 7. It is important that the patient start to breathe in as slowly as possible just before operating the inhaler. Practice in front of a mirror for the first few times. If the patient see “mist” coming from the top of the inhaler or the sides of the mouth, the patient should start again from stage 2.
If the doctor has given different instructions for using the inhaler, follow them carefully. Tell the physician if there are any difficulties.
Children: Young children may need help and an adult may need to operate the inhaler for them. Encourage the child to breathe out and operate the inhaler just after the child starts to breathe in. Practice the technique together. Older children or people with weak hands should hold the inhaler with both hands. Put the 2 forefingers on top of the inhaler and both thumbs on the base below the mouthpiece.
Cleaning: The inhaler should be cleaned at least once a week.
1. Remove the mouth piece cover.
2. Do not remove the canister from the plastic casing.
3. Wipe the inside and outside of the mouthpiece and the plastic casing with a dry cloth, tissue or cottonbud.
4. Replace the mouthpiece cover.
Do not put the metal canister into water.










Reviews
There are no reviews yet.